The avian flu virus isolated from a hospitalized teenager in Vancouver has mutations in key areas that could help the virus spread more easily in humans, scientists say.
There is no indication that the mutated virus has traveled beyond this patient. After monitoring of dozens of potential contacts among the teen’s friends, family and health care providers, “no further cases have been identified,” Dr. Bonnie Henry, provincial health officer for British Columbia, said in a written statement. That means the mutated virus is not spreading or a threat to anyone else.
But scientists say the genetic changes are a reminder of what the virus is capable of if it continues to spread.
“Certainly, this is one of the first times that we’ve really seen evidence of these sort of adaptation mutations in H5,” said Dr. Jesse Bloom, a computational virologist at the Fred Hutchinson Cancer Center.
The H5N1 bird flu virus that infected the teen, who is in critical but stable condition, is not the same strain that is transmitting in dairy cattle in the United States. It is more closely related to an H5N1 strain that is circulating in wild birds such as geese in the Pacific Northwest. Although both strains are H5N1, they are distinct, the same way Delta and Omicron were different versions of the SARS-CoV-2 virus that causes Covid-19.
Disease detectives who are investigating the case still don’t know how the teen was infected, since they had no known contact with wild birds.
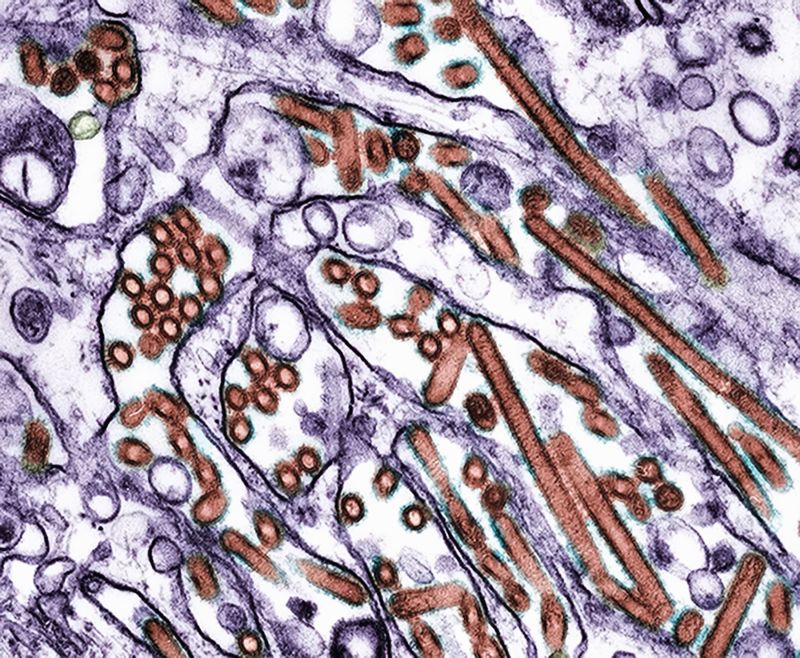
The three mutations are at positions in the virus’ genome that Bloom and other scientists have determined would allow it to attach more easily to human cells.
“It’s caught the attention of a lot of flu virologists, including myself, because some of the sequence has evidence of some of the types of mutations we worry about,” he said.
Flu viruses enter cells by attaching to sugars that stick up from their surfaces called sialic acids. Birds have an abundance of a kind of sialic acid called alpha 2,3, but humans primarily have alpha 2,6 sialic acids, particularly in the nose, throat and lungs.
Dr. Scott Hensley, a microbiologist and immunologist at the University of Pennsylvania who specializes in the study of flu viruses, says decades of basic research have shown scientists which mutations to watch for.
And Hensley said that on Saturday morning, when he looked up the sequence from the Canadian patient that had been newly uploaded to the international genome sharing database GISAID, he saw exactly the changes that would enable the virus to switch from preferring the alpha 2,3 receptor plentiful in birds to the alpha 2,6 sialic acids plentiful in the human nose, throat and lungs.
One place in the human body where alpha 2,3 receptors are plentiful is the eye, he said. Most of the human H5N1 infections reported in the United States have had red, inflamed eyes as an early symptom, suggesting that’s where the virus entered the body.
The Canadian youth also had red eyes as one of their first symptoms, so Hensley thinks it’s possible that’s how the virus got in. However, the patient developed severe breathing problems called acute respiratory distress syndrome, or ARDS, perhaps as a result of the mutations the virus began to acquire as it copied itself in the body, Hensley said.
Still, this is not the beginning of a pandemic, he stressed. The virus becoming better adapted to the human cells is a start, but it wouldn’t necessarily be enough on its own to ignite an outbreak.
“We need to do a lot of studies at this point. We have to try to understand if this particular virus does have properties of effective transmission,” he said.
Each of the mutations is ambiguous, meaning when scientists read the sequence of letters that make up the virus’ genome, they weren’t able to determine which of two letters, or nucleotides, should be in that position.
Bloom explains that this can happen when a virus is evolving in its host and present in the body in different forms.
“It’s commonly observed, when you look at sort of this sequencing of how a virus is evolving within a single host, that after an infection is gone for a couple of weeks, you’ll see a mix of different mutations,” he said.
The Canadian teen began having symptoms a week before they were admitted to the hospital, which may have been enough time for the virus to grow better at infecting the cells it was trying to enter.
- Sign up here to get The Results Are In with Dr. Sanjay Gupta every Friday from the CNN Health team.
Ambiguous mutations can also be a result of the sequencing itself, but Bloom doesn’t think that’s likely since the mutations don’t seem to be random and are instead at important positions where the virus would need to change to survive in its human host.
He notes that a number of H5N1 viruses isolated from infected birds in British Columbia and in Washington are closely related to this virus, but none has these particular mutations.
Although this seems to be a single dead-end infection – meaning it’s not going to spread beyond this person – it’s a good reminder that if the virus could do this once, it could do it again.
In the United States, 53 bird flu cases have been identified in humans and there are ongoing outbreaks in dairy cattle, sporadic outbreaks in poultry and widespread infections in wild birds.
“There’s a lot of H5N1 influenza out there,” Bloom said, “And influenza has a high mutation rate, so if this virus is in the right evolutionary space to acquire these mutations once, it’s possible – it’s not certain, but it’s possible – it could acquire them again in other infections.”